Heart Transplant Techniques Review: A Leap in Cardiac Care
In the field of cardiac care, heart transplant techniques have advanced greatly. Minimally invasive approaches offer reduced recovery times and complications with smaller incisions. Robotics aid in precision, while remote monitoring tracks progress. Organ matching algorithms reduce wait times, increasing donor heart availability. Enhanced post-transplant care includes better monitoring and patient education for improved outcomes. Donor organ preservation techniques and immunosuppressive therapies have evolved for better organ viability and rejection prevention. Matching artificial heart devices to patients efficiently and long-term monitoring strategies using wearable tech show promise. This innovation guarantees top-notch care and outcomes for cardiac transplant recipients.
Key Takeaways
- Minimally invasive approaches reduce recovery times and complications.
- Organ matching advancements decrease wait times for recipients.
- Enhanced post-transplant care improves monitoring and patient outcomes.
- Donor organ preservation techniques optimize organ viability.
- Immunosuppressive therapy innovations personalize drug regimens for better outcomes.
Minimally Invasive Surgical Approaches
When performing heart transplants, utilizing minimally invasive surgical approaches can greatly reduce recovery times and post-operative complications. These techniques involve smaller incisions, resulting in less pain and blood loss, faster healing, and shorter hospital stays.
Robotics assistance plays an important role in enhancing the precision and flexibility of these minimally invasive procedures. Surgeons can control robotic arms with high-definition cameras and specialized instruments, allowing for intricate maneuvers in tight spaces with improved accuracy.
Remote monitoring further complements these advancements by enabling healthcare providers to closely track patients' vital signs and recovery progress post-surgery. Through wearable devices and telemedicine, medical teams can intervene promptly if any issues arise, ensuring timely interventions and personalized care. This proactive approach significantly enhances patient outcomes and reduces the risk of complications during the critical post-operative period.
Organ Matching Advancements
Advancements in organ matching technologies have revolutionized the process of identifying suitable donors for heart transplant recipients. Donor selection is an essential aspect of heart transplant procedures, as compatibility between the donor organ and the recipient is vital for a successful outcome. With the evolution of organ matching advancements, transplant teams can now utilize sophisticated algorithms and databases to assess compatibility based on various factors such as blood type, tissue compatibility, organ size, and medical urgency.
Organ availability plays a significant role in the success of heart transplant procedures. The improved organ matching technologies have enabled medical professionals to expedite the matching process, leading to reduced wait times for recipients in need of a heart transplant. This efficiency in organ matching has helped increase the chances of finding suitable donor hearts within a shorter timeframe, ultimately saving more lives.
Improved Post-Transplant Care Protocols
When it comes to improved post-transplant care protocols, consider implementing enhanced monitoring techniques to track patient progress more effectively.
Engaging in patient education initiatives can also play an essential role in helping recipients actively participate in their own care post-transplant.
These strategies aim to optimize outcomes and enhance the overall quality of life for heart transplant recipients.
Enhanced Monitoring Techniques
To enhance post-transplant care protocols, implementing advanced monitoring techniques is crucial for guaranteeing excellent patient outcomes and early detection of potential complications. Utilizing remote monitoring systems integrated with wireless technology can provide real-time data on essential signs, medication adherence, and early warning signs of rejection or infection. These systems enable healthcare providers to track patients' progress outside of the hospital setting, allowing for timely interventions and adjustments to treatment plans.
Wireless devices such as wearable monitors and implantable sensors offer continuous monitoring capabilities, giving clinicians a detailed view of the patient's health status. Data collected from these devices can be transmitted securely to healthcare providers, facilitating proactive management of post-transplant care.
Furthermore, remote monitoring allows for increased patient autonomy and convenience, as individuals can perform self-checks and transmit data from the comfort of their homes. This proactive approach not only enhances patient satisfaction but also ensures that any deviations from the norm are promptly addressed, promoting better outcomes and reducing the risk of complications post-transplantation.
Patient Education Initiatives
Implementing patient education initiatives is vital for enhancing post-transplant care protocols and guaranteeing best patient outcomes. Patient education plays a critical role in improving adherence to medications, lifestyle modifications, and recognizing signs of complications post-heart transplant. By providing detailed information on medication schedules, dietary restrictions, and the importance of regular follow-up appointments, patients can actively participate in their care, leading to better long-term outcomes. Educating patients about potential complications such as rejection episodes and infections empowers them to seek timely medical intervention, ultimately impacting patient outcomes positively.
Furthermore, patient education initiatives contribute significantly to enhancing the quality of life for heart transplant recipients. Educated patients are better equipped to manage stress, cope with the emotional aspects of transplantation, and engage in appropriate physical activity, all of which are essential for improving their overall well-being post-transplant. By focusing on thorough patient education, healthcare providers can promote better patient outcomes and ensure a higher quality of life for individuals undergoing heart transplantation.
Enhanced Donor Organ Preservation Techniques
Enhanced techniques for preserving donor organs have revolutionized the field of heart transplants, ensuring peak organ viability and improving patient outcomes. Donor selection plays an essential role in obtaining high-quality organs for transplantation. Transportation logistics must be meticulously planned to minimize ischemic time and maintain organ integrity during transit.
- Hypothermic Machine Perfusion: Organs are cooled and perfused with a preservation solution to maintain viability.
- Normothermic Machine Perfusion: Organs are kept at body temperature to mimic physiological conditions and enhance preservation.
- Different Preservation Solutions: Tailored solutions are used to optimize organ preservation based on specific requirements.
- Subnormothermic Perfusion: Organs are perfused at slightly lower temperatures to reduce metabolic demand and prolong preservation time.
- Ex Vivo Heart Perfusion: Hearts are perfused and monitored outside the body to assess function and viability before transplantation.
These advancements in donor organ preservation techniques have significantly increased the success rates of heart transplants, providing new hope for patients in need of life-saving procedures.
Immunosuppressive Therapy Innovations
You're about to explore novel immunosuppression approaches that have revolutionized heart transplant outcomes. Enhanced rejection prevention strategies will be discussed, focusing on cutting-edge techniques to improve graft survival rates.
Additionally, personalized drug regimens tailored to individual patients will be highlighted for their potential in minimizing side effects while maximizing therapeutic benefits.
Novel Immunosuppression Approaches
Researchers have recently developed innovative immunosuppression approaches that show promise in improving outcomes for heart transplant recipients. These novel drug therapies aim to enhance the efficacy of immunosuppressive agents while reducing adverse effects. Some of the cutting-edge approaches include:
- Targeted Therapies: Utilizing medications that specifically target the immune cells involved in rejection processes, minimizing damage to healthy tissue.
- Biologic Agents: Introducing biological drugs that have a more targeted action on the immune system, potentially reducing the need for broad immunosuppression.
- Personalized Medicine: Tailoring immunosuppressive regimens based on individual genetic factors to optimize treatment outcomes.
- Drug Combination Strategies: Implementing unique combinations of immunosuppressive drugs to enhance efficacy and reduce the risk of rejection.
- Nanotechnology: Exploring the use of nanoscale drug delivery systems to improve drug targeting and reduce systemic side effects.
These advancements in immunosuppression hold great promise for revolutionizing post-heart transplant care by enhancing patient outcomes and quality of life.
Enhanced Rejection Prevention
Innovative immunosuppressive therapy advancements have shown significant potential in enhancing rejection prevention post-heart transplant. Rejection monitoring plays an essential role in this process, allowing healthcare providers to detect signs of rejection early on. By closely monitoring rejection risk factors, such as immune suppression levels and inflammatory markers, personalized therapy plans can be tailored to each patient's specific needs.
These advancements have enabled a more targeted approach to immune suppression, minimizing rejection risk while reducing the likelihood of adverse side effects. Immunosuppressive medications are now being fine-tuned based on individual patient characteristics, including genetic factors and immune response profiles. This personalized approach not only enhances rejection prevention but also improves overall transplant outcomes.
Personalized Drug Regimens
Utilizing cutting-edge pharmacogenomic insights, personalized drug regimens revolutionize immunosuppressive therapy for heart transplant recipients. By tailoring medications to individual genetic profiles, precision medicine offers a new level of care and effectiveness in managing post-transplant immunosuppression. Here are five key aspects of personalized drug regimens in heart transplant recipients:
- Individualized Dosing: Dosages are carefully calculated based on genetic factors, ensuring ideal drug levels for each patient.
- Genetic Compatibility Testing: Screening for genetic markers helps identify the most suitable immunosuppressive medications for the individual.
- Drug Interaction Monitoring: Continuous assessment of potential drug interactions helps prevent adverse effects and optimize treatment outcomes.
- Adverse Reaction Prediction: Genetic data enables the prediction of potential adverse reactions, allowing for proactive management strategies.
- Long-Term Efficacy: Personalized drug regimens promote long-term medication adherence and overall transplant success through tailored treatment plans.
Incorporating these personalized approaches into immunosuppressive therapy represents a significant advancement in enhancing outcomes for heart transplant recipients.
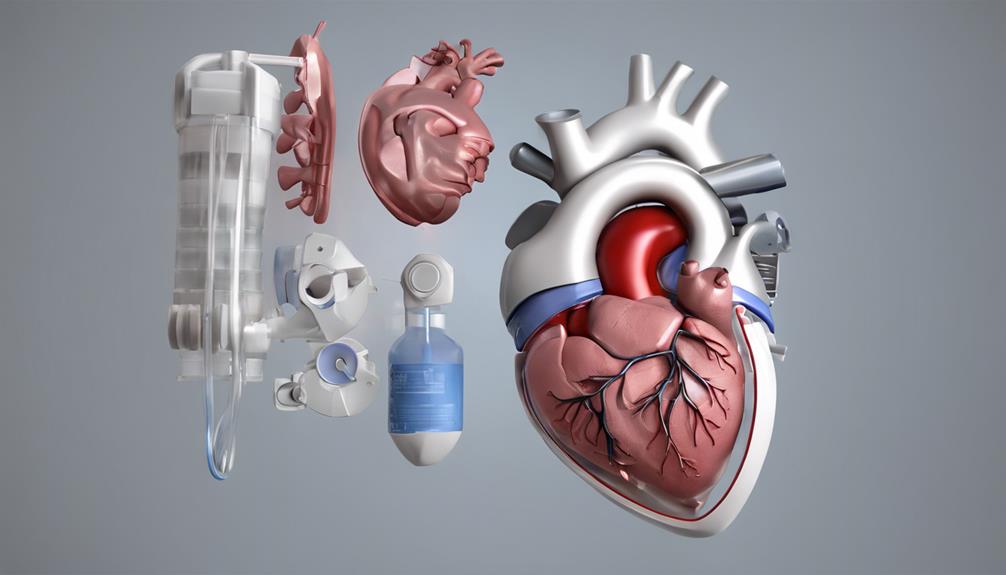
Artificial Heart Devices Integration
Incorporating artificial heart devices into existing transplantation procedures requires careful coordination and precise surgical techniques. The evolution of artificial heart development has paved the way for improved patient outcomes in cardiac care. Integrating these devices involves evaluating device compatibility with the recipient's anatomy and ensuring proper fitment to avoid complications.
One of the primary challenges faced during this integration process is the need to match the size and function of the artificial heart device with the recipient's cardiovascular system. Surgeons must meticulously plan and execute the implantation procedure to guarantee excellent performance post-transplantation.
Furthermore, ensuring the seamless integration of artificial heart devices necessitates a thorough understanding of the recipient's unique cardiac anatomy. Surgeons must navigate potential obstacles and adapt their techniques to accommodate individual variations.
Long-Term Patient Monitoring Strategies
Implement a thorough long-term patient monitoring strategy to track and manage post-transplant progress effectively. To guarantee the best care for heart transplant recipients, incorporating remote monitoring and telemedicine services is essential. These tools allow healthcare providers to keep a close eye on patients' health status without the need for frequent in-person visits, enhancing convenience and timely intervention.
Here are five key components of a robust long-term patient monitoring strategy:
- Regular Remote Monitoring: Utilize wearable devices to track vital signs and overall health status continuously.
- Telemedicine Consultations: Conduct virtual appointments to discuss any concerns or changes in the patient's condition.
- Medication Adherence Tracking: Implement systems to monitor medication intake and address any deviations promptly.
- Symptom Reporting Platforms: Enable patients to report symptoms in real-time for immediate medical attention.
- Data Analytics Integration: Utilize advanced analytics to identify trends and potential issues early on, allowing for proactive management.
Conclusion
You have now witnessed the transformative advancements in heart transplant techniques, propelling cardiac care into a new era of precision and efficacy.
With minimally invasive surgical approaches, organ matching advancements, improved post-transplant care protocols, enhanced donor organ preservation techniques, immunosuppressive therapy innovations, artificial heart devices integration, and long-term patient monitoring strategies, the future of heart transplants holds unprecedented promise.
Embrace the evolution in cardiac care and witness the unparalleled impact on patient outcomes.